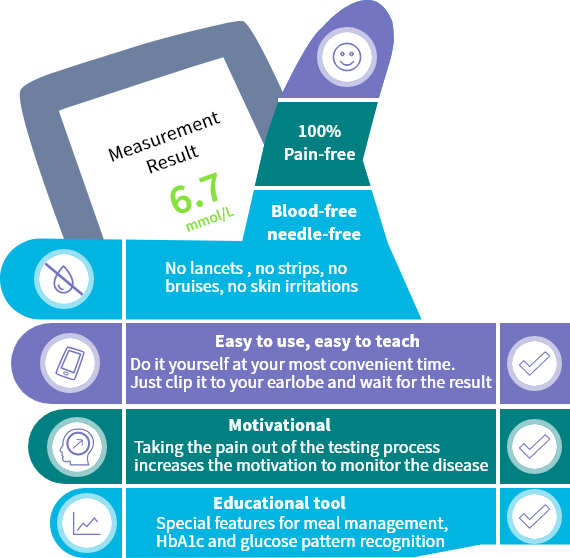
An innovative way to overcome barriers to glucose self-monitoring


Frequent glucose monitoring reduces HbA1c
For all types of diabetes and treatments 3
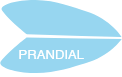
Adequate glycemic control reduces the risk of diabetes complications 4
HbA1c level is the gold-standard indicator
A new paradigm for assessing glucose profiles in the tissue
There is a high correlation found between glucose values measured with plasma gold-standard method and tissue glucose values measured with GlucoTrack, indicating that this is a reliable way to assess glucose profiles.
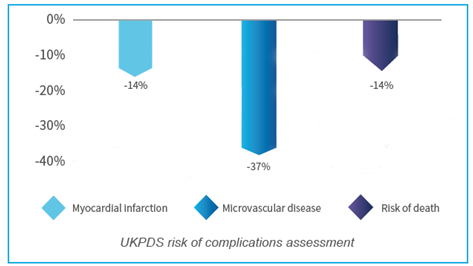
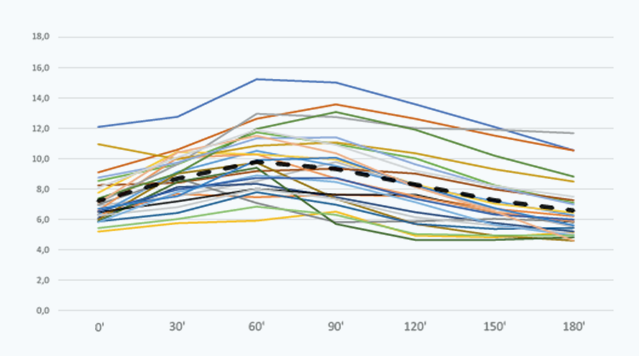
Plasma and tissue inter-patient glucose profile variability
 Time (min) elapsed after a meal
Time (min) elapsed after a meal
Plasma glucose (mmol/L measured with YSI)
 Time (min) elapsed after a meal
Time (min) elapsed after a meal
Tissue glucose (mmol/L measured with GlucoTrack)
Glucose concentrations in tissue show a general lagging effect in the post-prandial state compared with plasma values. Post-prandial time lag can be individually optimized.
“The lag time does in any case not compromise one of the main intentions for frequent non-invasive glucose measurement, which is to identify the right time for treatment initiation or intensification.”
(Prof. Dr. Andreas Pfützner, principal investigator of the clinical evaluation study)
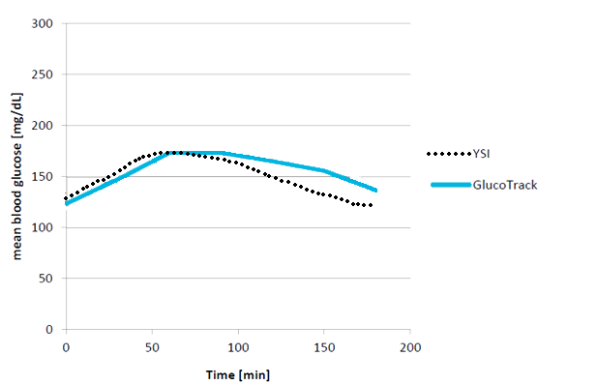
Tissue Glucose Time Lag vs Plasma
Evaluation of GlucoTrack® Model DF-F Non-Invasive Glucose Monitoring Device in Patients with Type 2 Diabetes and Subjects with Prediabetes.
Pfützner A. et al. Oct. 2016
The results confirm a stable GlucoTrack device performance among its intended users, including prediabetic patients, for frequent pain-free non-invasive monitoring of glucose levels.
Accurate and precise glucose results in pre and post-prandial states

GlucoTrack clinical validation compendium Dec 2018.
| 99.7% | of results in zones A+B6 (91.3% in Zone A) | |
| 7.9 ± 0.6 | Mean PARD ± SD7 | |
| 98.2% | of post-prandial results in zones A + B8 |
Performance of a non-invasive glucose monitoring device: accuracy and precisión
Sror M. et al. ATTD, 2018
GlucoTrack is highly accurate. Sensor-to-sensor precision is comparable to that of CGMs.
Non-Invasive glucose monitoring device: reducing impact of post-prandial lagging effect during measurement
Gal A. et al. DTM, 2016
Lagging effect correction equalizes accuracy for pre- and post-prandial readings.
Reliable and stable results over 6 months for a broad range of people with type 2 diabetes and prediabetes
Applicability of a non-invasive glucose monitor in subjects with various demographic profiles throughout 6 months of use
Gal A. et al. IDF, 2015
These findings suggest that the cost-effective, painless device is suitable for various type 2 diabetes population, for the entire calibration validity period.
Influence of medications on the accuracy of GlucoTrack® - a non-invasive glucose monitoring device
Lin T. et al. ADA, 2017
Clinical and numerical accuracies are comparable between all subjects regardless of tested medication consumption, indicating that GlucoTrack is suitable for subjects under medication regime.
The accuracy of a non-invasive glucose monitoring device does not depend on clinical characteristics of people with type 2 diabetes mellitus
Lin T. et al. January 2018
GlucoTrack performance does not depend on diabetes duration, HbA1c level, and smoking history, indicating the device is suitable for various people with type 2 diabetes.
What patients say about GlucoTrack

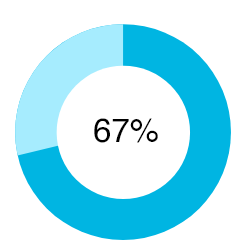
Pleased with the device
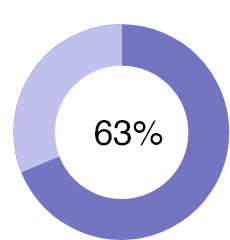
I will test more often
81% of patients who assessed GlucoTrack’s usability were pleased or very pleased with the device
- Fully Agree
- Tend to Agree
- Neutral
- Tend to Disagree
- Fully Disagree

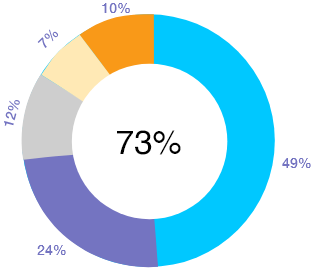
73% of patients declared their intention to monitor more frequently with GlucoTrack®
Acceptance of a Truly Non-Invasive Glucose Monitoring Device for Home Use
Gal A. et al. EASD, 2014
GlucoTrack maintenance of performances in home use regardless of user skills shows device suitability for layperson use.
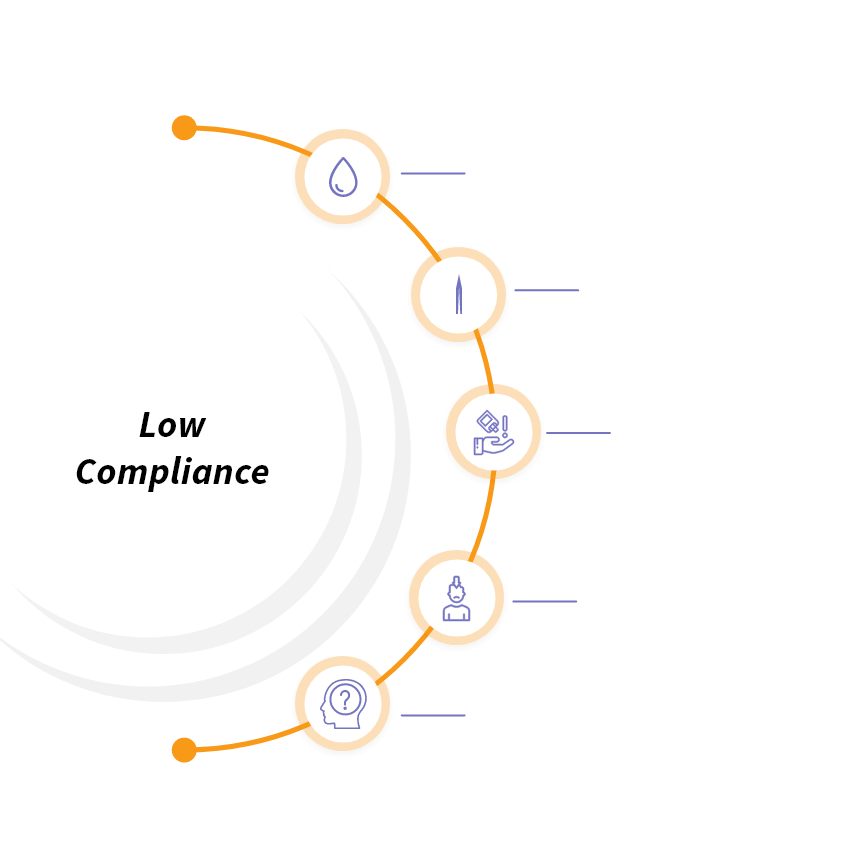
Which patients can benefit the most from using GlucoTrack?


Low compliance to self-monitoring blood glucose
Patients testing less frequent than recommended; patients naïve to glucose monitoring.

Need enhanced insights or greater motivation
When glucose values do not explain HbA1c levels ; patients about to move to the next therapeutic step; patients who need to test very often.

Resistance to invasive testing
Patients with anxiety or distress; fragile patients; afraid of finger pricking.
1 Karter AJ et al. Diabetes Care. 2000. 2 Wagner J et al. Diabetes Technology & Therapeutics. 2005. 3 Karter AJ et al. The American Journal of Medicine. 2001. 4 Stratton I et al. UKPDS. British Medicine Journal. 2000. 5 Leszeck C et al. Diabetes Technol Ther. 2014. 6 GlucoTrack clinical validation compendium Dec 2018. 7 Sror M et al. ATTD. 2018. 8 Gal A et al. DTM. 2016.